Home > PTTC Post Article - July 2019

Zili Sloboda, Sc.D.
President, Applied Prevention Science International
The United States has a long history of substance use problems which continue to pose challenges in spite of the progress made in treatment and prevention research. In particular, there has been an alarming rise in opioid use—both heroin and prescription painkillers--and significant consequences including overdoses and death (Rudd, et al., 2015). We are experiencing significant changes to the legal status of marijuana with implications that are difficult to predict. There is a clear need for research-based community-oriented policies and financial/organizational infrastructures to reduce the use and abuse of substances by children, and to reduce adult use of marijuana and other psychoactive substances in hazardous ways such as while driving (Azofeifa, et al., 2015)–or performing other sensitive activities.
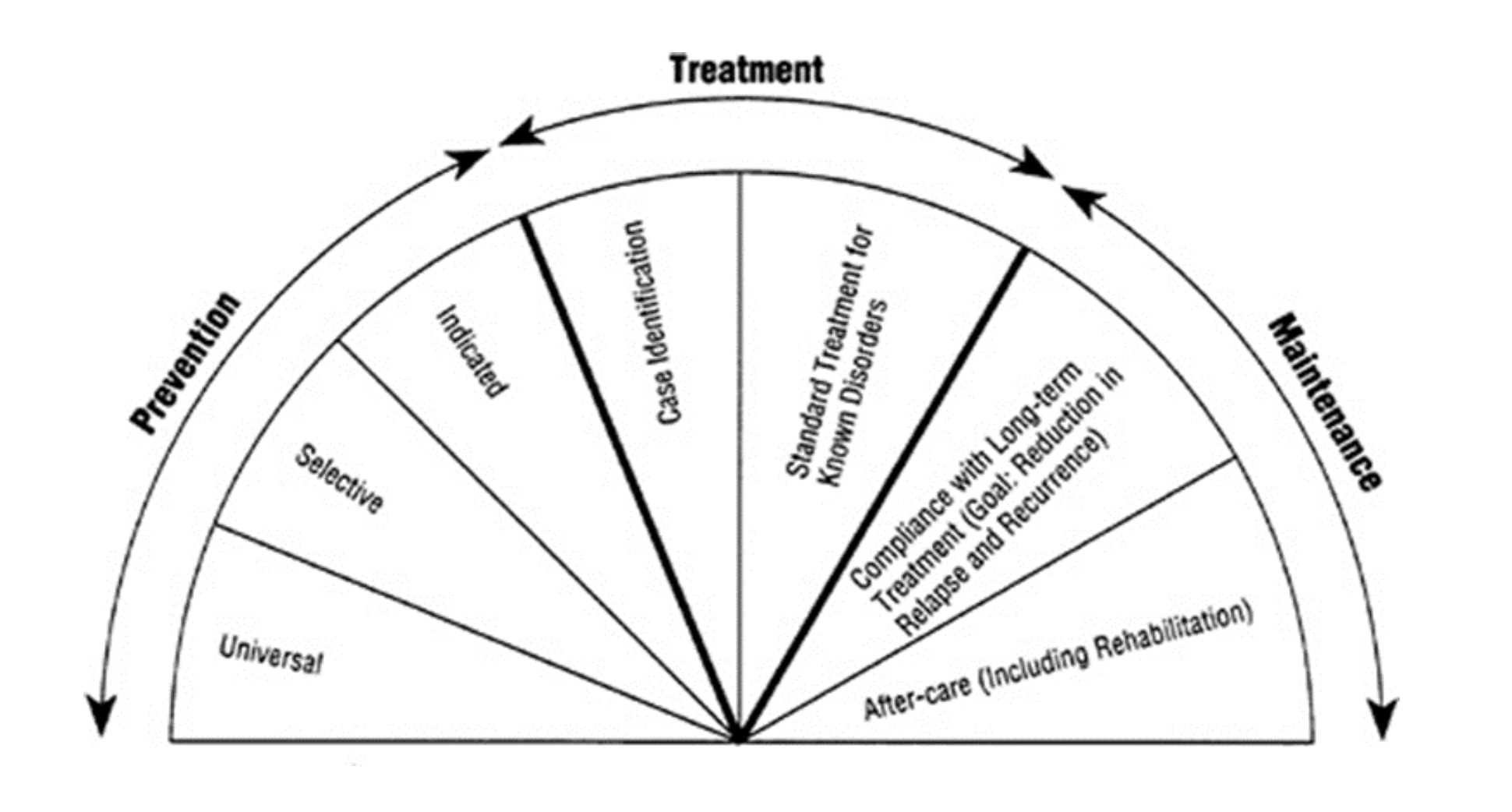
A particular concern is that funding for effective prevention programs is highly – and often exclusively - dependent on federal funding. This prevents local planning and jeopardizes the longevity and effectiveness in preventing substance use (NASADAD, 2016). Ending the fragmentation of community-based prevention and treatment programs and integrating them into one service-system will strengthen public health and safety service provision as these services would impact both the incidence (new cases) and the prevalence of substance use and abuse. However, achievement of this goal requires a more knowledgeable and professional workforce and a knowledge base and understanding about evidence-based programming, both of which are fundamental to building an effective community-based comprehensive infrastructure that can address local needs. Such a system would represent the spectrum of services put forward by the National Academy of Sciences (1994) shown below.
Among substance use professionals, there has been a consensus on several important needs:
The past 50 years have seen progress in understanding the etiology and epidemiology of substance use and in how to effectively prevent and treat substance use and substance use disorders. However, the implementation of effective prevention and treatment interventions are not taking place (e.g., D’Aunno et al, 2019; Frimpong et al., 2016 Ringwalt et al., 2008; Sloboda et al., 2008).
What is missing? Building a strong community-based infrastructure to support both prevention and treatment interventions that includes sustained funding, matching interventions to the needs of the community, tracking substance use trends within the community, continuous monitoring of intervention processes and assessments, and a well-trained, science-based prevention and treatment professionals IS needed. The objectives of this infrastructure are to:
How to move forward? The overlap between the regional Prevention Technology Transfer Centers and the Addiction Technology Transfer Centers provides an opportunity to move toward the goal of developing a national community-based integrated service delivery system for the prevention and treatment of substance use and substance use disorders based on evidence of effectiveness. The development and implementation of such a system would be a multi-staged process as outlined below.
Phase I—Problem Assessment and Framing the Elements of a Strategic Plan. Develop a planning group of approximately 25 leaders including substance use epidemiologists, prevention, and treatment researchers and practitioners, law enforcement, judiciary, schools, families, communities, policy makers, and health services who would meet to refine a model of a community-based integrated comprehensive substance use service delivery system, a summary of challenges to building such a system, and the initial framework for a strategic plan for developing demonstration systems that will be closely evaluated. The plan would include goals, objectives, performance outcomes, and key actions for successful implementation. The plan will also outline recommendations and implementation steps that would be funded from other sources.
Phase II—Expanded Stakeholder Involvement. The final draft comprehensive strategy will be disseminated to the public and an expanded team of experts to get input and support for a community-based integrated and comprehensive service delivery system and for the concept of demonstration projects. These additional planners will likely represent the public sector of Federal, state and local government and will be helping to forge implementation approaches.
Phase III—Develop Training and Technical Assistance Protocols to Professionalize the Prevention and Treatment Community. Working with universities and prevention and treatment specialists, this phase would help train substance use prevention and treatment professionals both through a degree program and through Continuing Education using the Universal Prevention Curriculum and the Universal Treatment Curriculum. Training would license individuals based on work experience and test scores with quality upgrades over time, help communities build an implementation system to support prevention and treatment to include health and social services, schools, parent groups, businesses, law enforcement and the judicial system.
Phase IV—Build Community-level Assessment systems. A comprehensive prevention and treatment system requires screening services and monitoring systems that link service needs with research-based programming.
Phase V—Identify a Model Community Prevention and Treatment Infrastructure. Communities will benefit from a guidance document drawing from the results of Phases I-III that delineates how to professionalize and implement a comprehensive prevention and treatment system. This would involve the development of a model representing the continuum of services that are recommended and the concept of supporting three or more demonstration sites that will be monitored and evaluated.
References:
Azofeifa, A., Mattson, M.E., & Lyerla, R. Driving under the influence of alcohol, marijuana, and alcohol and marijuana combined among persons aged 16-25 years – United States, 2002-2014. Weekly Morbidity and Mortality Report. December 11, 2015 / 64 (48); 1325-9.
D’Aunno, T., Park, S.E. & Pollack, H.A. (2019). Evidence-based treatment for opioid use disorders: A national study of methadone dose levels, 2011-2017. Journal of Substance Use Treatment, 96, 18-22.
Frimpong, J. A., D'Aunno, T., Helleringer, S., & Metsch, L. R. (2016). Low Rates of Adoption and Implementation of Rapid HIV Testing in Substance Use Disorder Treatment Programs. Journal of Substance Abuse Treatment, 63, 46-53. https://doi.org/10.1016/j.jsat.2015.12.001
Palamar, J. J., Shearston, J.A., Dawson, E.W., Mateu-Gelabert, P., & Ompad, D.C. (2016) Nonmedical opioid use and heroin use in a nationally representative sample of us high school seniors. Drug and Alcohol Dependence 158, 132-138.
Ringwalt, C., Hanley, S., Vincus, A.A., Ennett, S.T., & Rohrbach, L.A. (2008). The prevalence of effective substance use prevention. Journal of Primary Prevention, 29, 479-488.
Ringwalt, C., Vincus, A.A., Hanley, S., Ennett, S.T., Bowling, J.M., & Rohrbach, L.A. (2009). The prevalence of evidence-based drug use prevention. Prevention Science, 10, 33–40.
Rudd, R.A., Aleshire, N., Zibbell, J.E., & Gladden, R.M. Increases in drug and opioid overdose deaths – United States, 2000-2014. Weekly Morbidity and Mortality Report, January 1, 2016/64(50); 1378-82.
Sloboda, Z., Pyakuryal,A., Stephens, P., Teasdale, B., Forrest, D., Stephens, R.C., Grey, S.F. (2008). Reports of substance abuse programming available in schools. Prevention Science. 9(4), 276-87